VISION: The best care for every baby, every family, every time.
MISSION: We will provide compassionate, quality care and catalyze impactful research, education, and advocacy to improve outcomes for newborns everywhere. We do this within an inclusive community that cultivates diverse teams to do meaningful work.
VALUES: Collaboration, Curiosity, Dignity, Equity, Integrity
About
The Division of Neonatology at the University of Washington began in the early 1960s with the establishment of the region’s first organized programs dedicated to the care of critically ill newborns. Dr. W. Alan Hodson guided the Division through its formative decades, building a collaborative clinical model to deliver advanced neonatal care.
Throughout the 1970s and 1980s the Division expanded its fellowship program, strengthened partnerships with obstetrics and pediatric subspecialties, and helped shape regional perinatal systems of care. Clinical innovation, including early respiratory support strategies and transport capabilities, positioned the Division as a leader in caring for high-risk infants in the Pacific Northwest.
In the 1990s and 2000s, new leadership broadened the Division’s mission to include educational innovation, simulation-based training, and multidisciplinary quality improvement. The Division also maintained a strong research presence that advanced understanding of neonatal physiology and neuroprotection.
Today, the Division provides neonatal care across ten NICUs, trains the next generation of neonatal clinicians, and leads practice improvement efforts across the region. Its history reflects a long-standing commitment to clinical excellence, education, and discovery in service of newborns and their families. As the Division has grown, so has our sphere of research interests, and these now include global neonatal‐perinatal health, health professional simulation, pulmonary physiology and ethics.
Neonatal Intensive Care Units
- University of Washington Medical Center-Montlake Neonatal Intensive Care Unit (Level IV)
Kirti Upadhyay, MD, Medical Director
Sarah Kolnik, MD, MBA, Medical Director
Tiffany Stanley, ARNP,, NNP Program ManagerThe UWMC NICU admits critically ill newborns from one of the highest risk obstetric services in the nation. The multi‐professional perinatal and NICU teams have special expertise in management of the most fragile growth‐restricted and extremely premature fetuses and newborns. The high‐risk perinatal program receives obstetrics referrals from throughout the WWAMI region for fetal abnormalities, severe maternal illness, and extreme prematurity and is the site of delivery for the most complex birth defects, including infants requiring EXIT procedures for airway anomalies. Additional advanced services include therapeutic hypothermia and the full range of ventilation strategies including inhaled nitric oxide, high –frequency oscillatory and jet ventilation. The NICU medical team includes neonatal faculty, neonatal fellows, neonatal nurse practitioners, neonatal hospitalists, pediatric residents, interns and medical students. The inter‐professional team includes dedicated respiratory therapists, neonatal pharmacists, dieticians, physical therapists, speech language pathologists and social work support. The nursing team includes three tiers of RN expertise and leadership. A state‐of‐the‐art 50‐bed NICU opened October 2012. The NICU includes 42 single‐bed rooms with space for a family member to stay with their infant plus several additional rooms for multiples as well as an integrated OR for surgical procedures. Patients are cared for by one of two multi‐disciplinary teams, a resident‐based team, and an NNP/hospitalist team. The UWMC NICU’s care model includes 24/7 coverage by in‐house residents and, mid‐level intensivists (fellow or NNP/PA), under the direction of attending neonatologists. In 2020, the UWMC had 1961 deliveries with 469 NICU admissions. The average daily census was 28 with 17 preterm infants weighing less than 1500 grams at birth and an average daily census of 1.6 on ventilators.
- Seattle Children’s Hospital Neonatal Intensive Care Unit (Level IV)
Zeenia Billimoria, MD, Medical Director
April Morris, MN, ARNP, Director, Advance Practice Services
Melissa Koll, MN, ARNP, Supervisor of SCH NICU APPs
Mihai Puia-Dumitrescu, MD, MPH, CMQ, Assoc. Medical Director
Sarah Handley, MD, Assoc. Medical Director
The Neonatal Intensive Care Unit at Seattle Children’s Hospital is the highest rated Level IV NICU in the Seattle area and serves as the major quaternary referral center for medically and surgically complex neonates in the Pacific Northwest. Seattle Children’s NICU admits 500 patients annually and has over 500 affiliated faculty that represent all pediatric subspecialties including– more than any other hospital in the region. The Children’s NICU provides the full spectrum of neonatal medical care including therapeutic hypothermia for acute hypoxic ischemic encephalopathy, seizures, high frequency ventilation, inhaled nitric oxide and ECMO for severe respiratory failure, renal replacement therapy including dialysis and surgical expertise in the areas of congenital diaphragmatic hernia, intestinal failure, bowel atresia, craniofacial anomalies, reconstructive pelvic medicine, post‐hemorrhagic hydrocephalus, neural tube defects and neurovascular malformations. In addition, we offer multidisciplinary care teams providing neuro‐critical care, congenital diaphragmatic hernia and management of bronchopulmonary dysplasia.Daily rounds with the medical team incorporate the patient’s family, NICU nurses, dieticians, pharmacists and respiratory therapists. The NICU team accepts admissions of critically ill neonates up to 44 weeks’ post menstrual age from the 5‐state WAMI region. The Seattle Children’s Hospital NICU’s care model includes an in‐house fellow or NNP and attending neonatologist 24/7. Seattle Children's Prenatal Diagnosis and Treatment Program partners with the University of Washington to provide care for pregnant women and their families when pregnancy is complicated by known or suspected conditions in the developing fetus. Our program integrates obstetric, neonatology and pediatric specialty care for families facing complicated pregnancy management or decision‐making. Seattle Children’s NICU participates in research and quality improvement initiatives via its active participation in a number of national and/or international collaborative associations including the Children’s Hospital Neonatal Consortium, Congenital Diaphragmatic Hernia Study Group, Bronchopulmonary Dysplasia Collaborative and the Extracorporeal Life Support Organization.
- UW Medicine/Valley Medical Center Neonatal Intensive Care Unit (Level III)
Christina Long, DO, Medical Director
Toby Cohen, MD, Assoc. Medical Director
Carol Otto MSN, ARNP, Supervisor, Valley Medical CenterIn July 2017, Neonatologists and Advanced Neonatal Practitioners from University of Washington/Seattle Children’s Hospital began a collaborative effort to staff the NICU at UW/Valley Medical Center. The unit has a 29‐bed capacity. The single‐bed rooms provide space and privacy for our patients and their families. Two, unique, infant stabilization rooms allow immediate resuscitation of infants in the NICU after birth without requiring transport after stabilization. Valley has a robust high‐ risk perinatal clinic and the Neonatologists work closely in conjunction with the high‐risk team to provide consults for families prenatally. The Valley NICU uses a multi‐disciplinary approach to patient care with NICU dedicated pharmacists, dieticians, physical therapists, speech therapists, respiratory therapists, social work, and NICU nurses. This multi‐disciplinary staff meets with families to provide the best family‐centered care for our patients. Advanced services provided at Valley include therapeutic hypothermia with 24/7 Pediatric Neurology support and a large range of ventilation strategies including high‐frequency oscillatory ventilation. Advanced Neonatal Practitioners staff the NICU with 24/7 in‐ house coverage under the direction of attending Neonatologists. In AY 2018, Valley had 3474 number of deliveries with 212 NICU admissions.
- Providence Regional Medical Center Everett Neonatal Intensive Care Unit (Level III)
Michael D. Neufeld, MD, MPH, Medical Director
Maya Kaneyasu, BSN, MN, ARNP Supervisor, Providence Regional Medical Center EverettProvidence Regional Medical Center Everett’s 29‐bed capacity NICU opened on Mother’s Day in 2002. The unit was developed through the efforts of an alliance between PRMCE and Seattle Children’s Hospital. Individual rooms provide privacy for patients and their families. The multidisciplinary team meets daily with parents and concentrates on family‐centered care, teaching parents how to take care of their infants, especially those with special needs. In preparation for discharge, parents are provided in‐depth instruction on how to manage emergencies that may arise in the home, including the need for CPR. The unit cares for infants of all gestational ages and has HFJV, HFOV, and iNO in addition to conventional ventilation. The care model at PRMCE is 24/7 in‐house Advanced Neonatal Practitioners and Physician Assistants under the direction of an attending neonatologist. In AY 2020, PRMCE had 4162 deliveries with 588 NICU admissions. The average daily census was 23.5 with 59 preterm infants weighing less than 1500 grams at birth.
- Virgina Mason Franciscan Health; St Joseph Medical Center (Level III); St Francis Hospital (Level II); St Michael Medical Center (Level II); St Anne Hospital (Level II); Virginia Mason Medical Center (Level II)
Robin LaGrandeur, MD - Interim Medical Director St Joseph NICU and VMFH Neonatology Service Line
Krista Birnie, MD - St Anne SCN Medical Director
Angel Rios, MD - VMMC SCN Medical Director
Justine Wood, ARNP, NNP-BC, Neonatal APP Supervisor VMFHFranciscan Health Care System includes a network of hospitals with approximately 9,000 deliveries annually at its 5 obstetrical facilities: St Joseph Medical Center in Tacoma, St Francis Hospital in Federal Way, St Elizabeth Hospital in Enumclaw, St Michael Medical Center in Silverdale, and St Anne Hospital in Burien. St Joseph Medical Center has a licensed capacity of 34 neonatal beds and has 24/7 in‐house Advanced Neonatal Practitioners supported by faculty neonatologists. St. Francis Hospital has a licensed capacity of 10 Level II beds that receive medical care from local pediatricians, with consultation and attendance at high‐risk deliveries as needed from SCH Advanced Neonatal Practitioners and/or neonatologists. For 12 hours/day, Saint Francis has in house coverage with the Advanced Neonatal Practitioners with support from Neonatology Providers and for the other 12 hours/day, Neonatology provides coverage directly and via telemedicine. St Anne Hospital has a licensed capacity of 5 Level II beds, with inpatient Level II care and consultative services provided by Seattle Children’s Neonatologists on call. St. Elizabeth is a critical access hospital with 345 deliveries a year. Seattle Children’s Hospital partnered with the Franciscan Health Care System to begin providing Neonatology services and medical direction on April 1, 2013, and St. Joseph Medical Center opened its new Level III NICU in June 2013, and St Anne Hospital began its collaboration with Seattle Children’s in November 2018. This partnership has made it possible for the vast majority of patients to stay within their community while receiving excellent care for their fragile newborns. On 1/22/18, we lowered the gestational age at which we would manage patients at SJMC to 25 weeks as our threshold of care at SJMC. With the continued emphasis on non‐invasive ventilation as our primary mode of respiratory support, we average between 4 and 6 babies on nasal CPAP per day and less than one baby per day on invasive ventilatory support. In September of 2018, we expanded our care to provide inhaled nitric oxide for infants with hypoxic respiratory failure and we utilized it on three patients with excellent clinical responses. In AY 2018, St. Joseph’s had approximately 4100 deliveries with 480 NICU admissions. Our average daily census was 17.0 with 44 premature infants weighing less than 1500 and 14 weighing less than 1000 grams at birth.
- University of Washington Medical Center - Northwest Neonatal Intensive Care Unit (Level II)
Angel Rios, MD, Pediatric Section Head
In November of 2018 Northwest Hospital Special Care Nursery, a Level II NICU began a collaborative effort with the UW Division of Neonatology and Seattle Children’s Hospital to support care for infants born prematurely at greater than 32 weeks, as well as term infants who may be suffering from a variety of neonatal conditions including but not limited to breathing difficulties and infections. Northwest Hospital delivery service sees approximately 1100 newborn infants annually. Although historically the service delivers primarily low risk patients there is always the potential need for the expertise provided by 24/7 in house coverage by our team of Advanced Neonatal Practitioners who have immediate access to consultation with UW/SCH neonatologists and a premier critical care neonatal transport system. The unit is being remodeled to support the focus on family centered care with increased opportunity and available space for couplet care.
Clinical Programs
- Neonatal Consultation and Transport Program
Zeenia Billimoria, MD, Medical Director; Christopher Baker, MSN, MBA, RN C-NPT, Clinical Manager
The Division provides 24/7 neonatal consultation services for the 5-state WWAMI region. Neonatal transport services for Seattle Children’s and its affiliated hospital partners is provided by dedicated teams from Seattle Children’s and Airlift Northwest. Our transport team are leaders in safe newborn transport and have ground, rotor and fixed wing capability. Teams are comprised of specially trained transport nurses and respiratory therapists. Infants from referral centers throughout the WWAMI (Washington, Wyoming, Alaska, Montana, and Idaho) region are transported to Seattle Children’s. Services provided include various modes of non-invasive support, high frequency ventilation, administration of nitric oxide, blood gas analysis and mobile extracorporeal membrane oxygenation for critically ill patients too unstable to move via conventional support.
- Telemedicine Program
Rachel Umoren MBBCh, MS, Inpatient Medical Director for Telehealth
Core Team: Chris Cooper, Craig Jackson, Megan Gray, Taylor SawyerSince 2019, a dedicated neonatal telehealth team staffed by trained neonatologists and advanced practice providers has provided neonatal teleconsultation services including telerounding, teleconsultation and teleresuscitation.
- Prenatal Diagnosis Programs
Prenatal Diagnosis and Treatment Program at Seattle Children’s Hospital
Craig Jackson, MD, MHA; Robert DiGeronimo, MD, and Zeenia Billimoria, MD
This multidisciplinary clinic is held Monday through Friday in the Springbrook office center which is across the street from the main hospital. Patients are referred from Washington, Alaska, Montana, and Idaho. More than 1000 patients are seen annually for fetal imaging with ultrasound, echocardiogram, and MRI, and for multidisciplinary counseling by our UW maternal‐fetal medicine specialists, pediatric medical and surgical specialists, prenatal nurses, and by our genetic counselor and prenatal social worker. About half of the visits are for fetal cardiac evaluation for known or suspected fetal cardiac defects such as ductal‐dependent cyanotic heart disease, fetal arrhythmias, or for maternal health risk factors for fetal congenital heart disease. The remainder are referred for suspected fetal surgical problems (e.g., congenital diaphragmatic hernia, congenital pulmonary airway malformations, gastroschisis), neurodevelopmental disorders (e.g., open neural tube defects, ventriculomegaly), renal or urologic problems (e.g., urinary tract obstruction, renal dysplasia), and genetic issues (e.g., trisomy 13, 18, and 21 and numerous specific genetic conditions). Neonatologists are asked to join the multidisciplinary counseling for patients with fetal conditions that are complex, likely to require advanced delivery room resuscitation or admission to SCH, or which raise the possibility of offering palliative care. Research projects during 2020 included the following:
Principle Investigator Project Title Bhawna Arya Fetal anatomy and physiology and associations with fetal and perinatal outcomes in DTGA/IVS: a collaborative, multicenter, multi-arm prospective study Hannah Tully, Dan Doherty “Retrospective Review of Prenatally Diagnosed Fetal Central Nervous System Abnormalities” Aarti Bhat Prenatal detection of HLHS and dTGA: significant socioeconomic and geographic barriers Kiana Siefkas Biallelic SCN5A Variants Cause Prenatal Onset of Complex Cardiac Arrhythmias Bhawna Arya, Kim Riehle Utility of maternal hyperoxygenation testing in predicting outcomes in fetuses at risk for developing PPHN Bhawna Arya Prenatal predictors of coarctation of the aorta Bhawna Arya, Mikki Clouse Cerebral Doppler pattern in coarctation of the aorta Bhawna Arya Fetal predictors of PAIVS outcomes Bhawna Arya Fetal predictors of mitral valve dysplasia outcomes Bhawna Arya Umbrella IRB for fetal CHD retrospective studies Ian Glass Donation of Embryonic & Fetal Tissue for Research (BDRL) Daniel Doherty NDV Disorders & Hindbrain Malformations William Walker Evaluation of the Best Urologic Management for Newborns and Young Children with Spina Bifida Elizabeth Caris Resiliency in Families affected by Congenital Heart Disease Bailey Brinks Prenatal Tour Study: Evaluating Newborn Hospitalization Preparedness In Families With Prenatal Diagnosis Prenatal Diagnosis Program at University of Washington Medical Center
Craig Jackson, MD, MHA; Dennis Mayock, MD; Maneesh Batra, MD, MPH; and Davia Loren, MD
This clinic is held in the Maternal Infant Care Center (MICC) at UWMC where maternal‐fetal medicine specialists primarily see patients with suspected or known fetal defects for close monitoring during pregnancy, with ultrasound and non‐stress tests as needed, and genetic testing as appropriate. Neonatologists are asked to counsel patients with fetal defects about a month before the expected delivery of newborns who are at risk of needing admission to the UWMC NICU or be transported to Seattle Children’s Hospital. They also see pregnant patients with hypertension, multiple‐gestation, diabetes, and high‐risk for prematurity. Palliative care consultation from the UWMC NICU palliative care physician is available as needed. Current research projects include:
- Establishing growth curves for gastroschisis
- Prenatal bowel dilation in gastroschisis: predictors for timing of delivery and outcome
- cfDNA and maternal-fetal trafficking studies
- Neuro-NICU Program
Ulrike Mietzsch, MD, - Neonatal Co-director; Nina Natarajan, MD – Pediatric Neurology Co-director
The neonatal neurocritical care program at Seattle Children’s Hospital is a specialized service to improve the care and outcome of critically ill newborns with neurological and/or neurosurgical problems diagnosed in or before the newborn period. This advanced care service provides multidisciplinary care from experts in Neonatology, Neonatal Neurology, Neurosurgery, Pediatric Neuroradiology, Pediatric Neurophysiology, Neurogenetics, Developmental Pediatrics, Occupational & Physical therapists, audiologists and speech/language pathologists.
Conditions treated: Hypoxic ischemic encephalopathy (HIE)/birth asphyxia, Neonatal seizures, Brain malformations, Neonatal stroke, Metabolic encephalopathy, Meningitis/Encephalitis, Neuromuscular disorders, Hydrocephalus, Intracranial hemorrhage, White matter injury (PVL or diffuse), ECMO monitoring, Myelomeningocele.
Services provided: 24-hour continuous video monitoring – including electrophysiologists specialized in neonatal EEG, Whole-body hypothermia therapy, Active hypothermia during neonatal critical care transports (air and ground), Near-Infrared Spectroscopy Monitoring, Magnetic resonance imaging and spectroscopy, Neonatal EMG testing, Advanced neurogenetic diagnostics, Specialized small-baby care bundles, Comprehensive multidisciplinary High-Risk Infant Follow Up program including General Movement Assessment.
Approximately 30‐40% (~180 patients) of patients admitted to the Level IV NICU at Seattle Children’s Hospital receive supplemental care through the NeuroNICU service annually. In addition, a close collaboration has been established between the NICU at UW Medical Center and the NeuroNICU at Seattle Children’s in addition to referrals and consultations from the entire State of Washington, Idaho, Montana, and Alaska, for which the NeuroNICU team is providing consultation and outreach services.
- Infant Development Followup-up Clinic
Emily Myers, MD; Kendell German, MD; Nina Natarajan, MD
The University of Washington Institute on Human Development and Disability offer the Infant Development Follow‐Up Clinic (IDFC) and the Late and Moderate Preterm Baby Clinic (LAMBs) to provide interdisciplinary neurodevelopmental assessments for infants at risk for developmental differences. Infants receive standard evaluations at 3, 9, 12, 18, and 24 months, then annually through 5 years old. Developmental Pediatrics, Neonatal Neurology, Neonatology, Advanced Practice Nursing, Psychology, Speech/Language Pathology, Audiology, Nutrition, Occupational Therapy, Physical Therapy and Social Work staff the clinic. The clinic sees approximately 2500 infants and children annually. The clinic also provides interdisciplinary training and follow‐up for patients in clinical research studies.
Infants who qualify to be seen in these clinics are those that meet any of the following criteria:
- Infants born before 37 weeks’ gestation
- Birthweight of <1500g
- Infants exposed in-utero to drugs or alcohol
- Infants with prenatal, perinatal, or neonatal brain injuries (IVH, HIE, stroke)
- Infants with complex medical disease requiring selected surgical interventions
- Infants who required a neonatal intensive care unit hospitalization
Recent changes to these clinics include the introduction of the Reach Out and Read program and telehealth services which were employed during COVID restrictions. Ongoing research in the clinic includes follow‐up for the HEAL trial, the evaluation of the Reach Out and Read program in the NICU and follow‐up clinics and the creation of a patient database to facilitate quality improvement and outcomes research.
- Neonatal-Perinatal Clinical Collaboratives
Vermont-Oxford Network
Michael D. Neufeld, MD, MPH; Thomas P. Strandjord, MD, Database Coordinators
The University of Washington Medical Center Neonatal Intensive Care Unit maintains a quality improvement and research NICU database that includes all infants admitted to the NICU, as well as all infants delivered at UWMC over 22 weeks' gestation. The database is maintained by Division staff and faculty. In addition, since 2000, the University of Washington NICU has participated in the Vermont‐Oxford Network (VON) database for 401‐1500‐gram infants. Data is selected for inclusion in the NICU database by consensus of the neonatology faculty and fellows. The NICU database contains a superset of the data required by the VON database and as such includes extensive admission, diagnostic, outcome and local QA/QI data. The outcome (morbidity and mortality) data are generated annually and reviewed with the faculty and fellows. In addition, ad hoc queries are performed at the request of fellows and faculty and reviewed as a group.
Children’s Hospital Neonatal Consortium
Elizabeth Jacobson, MD, Site Physician Sponsor; Robert DiGeronimo, MD, Co-Sponsor
Seattle Children’s Hospital belongs to the Children’s Hospitals Neonatal Consortium (CHNC) of 40 children's hospital Level IV NICUs. This allows for involvement in benchmarking, quality evaluation, and improvement initiatives for the SCH NICU through the Children’s Hospitals Neonatal Database and focus groups on specific diagnoses, such as severe bronchopulmonary dysplasia, congenital diaphragmatic hernia, and hypoxic‐ischemic encephalopathy. Many of our neonatal faculty are members of one or more of the CHNC’s focus groups, including those mentioned as well as Fetal Therapy, ECMO, Necrotizing enterocolitis, Resuscitation, and Neurosurgery. In addition, Elizabeth Jacobson co‐leads the CHNC’s national Gastroschisis Focus Group. Publications from these efforts are listed in the Translational, Clinical, and Quality Improvement Research section of this Annual Report.
Extracorporeal Life Support Organization
Robert DiGeronimo, MD, Site Physician Co-Sponsor
Seattle Children’s Hospital belongs to the Extracorporeal Life Support Organization (ELSO), an international non‐profit consortium of over 350 health care institutions dedicated to the development and evaluation of novel therapies to support organ failure. Participation in ELSO affords the opportunity to participate in and query the extracorporeal membrane oxygenation database to support clinical research, quality improvement and evidence‐based guideline recommendations.
National Airway Registry for Neonates (NEAR4NEOS)
Taylor Sawyer, DO, MEd, Site Lead UWMC and SCH, Shilpi Chabra, MD, UWMC Site Co-Lead; Mihai Puia-Dumitrescu, MD, MPH, SCH Site Co-Lead
Both the University of Washington NICU and the Seattle Children’s Hospital NICU belong to the National Airway Registry for Neonates (NEAR4NEOS), an international collaboration of 16 academic neonatal intensive care units dedicated to improving the safety of neonatal intubation. Participation in NEAR4NEOS affords the opportunity to participate in clinical research and quality improvement projects around neonatal intubation.
- Regional Neonatology Outreach Program
Taylor Sawyer, MD
The Division of Neonatology Regional Outreach program started around 1980 when the WA State Department of Health received matching federal funds for regionalization of OB and neonatal services into four centers, including the University of Washington. The UW program split into OB at UW Medical Center and neonatal at Seattle Children’s Hospital (SCH) in about 1990. After federal funding for the program ended in about 2000, SCH continued to support a neonatal educator salary until about 2010 to do needs‐assessments for referring hospitals and to teach NRP. By then, most level II and III NICUs had their own clinical nurse specialists or educators. Our neonatal outreach program initially focused on addressing the training needs of level I and II delivery hospitals, and then helped interested level II centers become level III centers. In the early 1990s, SCH began to build more durable referral relationships through LLC arrangements and neonatal/pediatric hospitalist service contracts. In the early 2000s, SCH hired a neonatologist for the level III NICU at Kadlec (until they partnered with Prov‐Sacred Heart a few years later). The neonatology outreach leader began frequent trips to sites in central WA and western MT to build personal relationships, primarily by giving didactic presentations requested by the neonatologists and reviewing the outcomes of neonatal patients they sent to SCH or UW with brief educational comments. In about 2010, our neonatology outreach program expanded to include our level III/IV NICU medical directors. We meet regularly with SCH Neonatology director Jake Hawksworth and leaders in the SCH Strategic Planning and Business Development office. In 2019, we worked with them to develop a contract to support neonatal training services in Bozeman, MT.
Our division faculty have research focused on neuroscience, medical education, global neonatal-perinatal health, and ethics.
Research Programs
- Neonatal Neuroscience
Our Neonatal Neuroscience Program is focused on improving the neurodevelopmental outcomes of high‐risk infants. Components of our program include the Neonatal
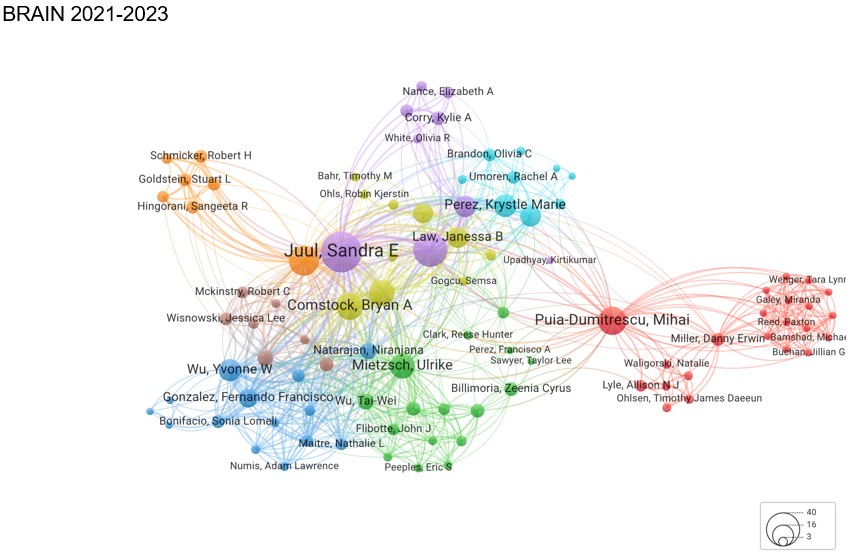 Neuroscience laboratory in which we carry out basic science studies to better understand mechanisms of brain injury and repair in a variety of neonatal brain injury models (rodents, ferrets and nonhuman primates), and the Brain Research Advancement in Neonatology (BRAIN) team which targets interdisciplinary clinical and translational research.
Neuroscience laboratory in which we carry out basic science studies to better understand mechanisms of brain injury and repair in a variety of neonatal brain injury models (rodents, ferrets and nonhuman primates), and the Brain Research Advancement in Neonatology (BRAIN) team which targets interdisciplinary clinical and translational research.Core Programs
- Neonatal neuroscience laboratory (NNL)- Sandra Juul, Tommy Wood, Janessa Law, Daniel Moralejo, Kylie Corry
- Brain Research Advancement in Neonatology (BRAIN) Team- Janessa Law, Tommy Wood, Mihai Puia-Dumitrescu, Kendell German, Krystle Perez, Ulrike Mietzsch
- NeuroNICU- Ulrike Mietzsch, Nina Natarajan, Jason Hauptman, Sandra Juul, Francisco Perez, Dennis Shaw, Hannah Tully, Mark Wainwright, Emily Myers
- Infant Development Follow-Up Clinic (IDFC)/Late and Moderate Preterm Babies Clinic (LAMBs)- Emily Myers, Nina Natarajan, Kendell German
- Neuroscience Fellowship Track- Sandra Juul, Nina Natarajan, Dennis Mayock, Kendell German, Janessa Law, Mihai Puia-Dumitrescu, Ulrike Mietzsch, Megan Gray, Thomas Wood
- PENUT and HEAL Data Coordinating Center (DCC)- Patrick Heagerty, Bryan Comstock
- Eunice Kennedy Shriver Intellectual and Developmental Disabilities Research Center (IDDRC)- Michael Guralnick, Sandra Juul
- Biomedical Image Computing Group- Todd Richards, Manjiri Dighe
Ongoing Trials and Collaborations
- Preterm Epo Neuroprotection (PENUT) trial- Sandra Juul, Patrick Heagerty, Dennis Mayock, Bryan Comstock
- High-dose Erythropoietin for Asphyxia and Encephalopathy (HEAL)- Sandra Juul, Patrick Heagerty, Dennis Mayock, Bryan Comstock
- Washington study of Outcomes, Neural Development and Early Risk (WONDER)- Frederick Shic, Sara Webb, Dennis Mayock
- Neonatal Education and Simulation-based Training (NEST) Program
Rachel Umoren, MBBCh, MS, Program Director, Co-Director of Research; Megan M. Gray, MD, Co-Program Director, Director of Research; Taylor Sawyer, DO, MBA, MEd; Zeenia Billimoria, MD, Director of Transport Simulation; Sarah Handley, MD, Director of ECMO Simulation; Chris Cooper, ARNP, NNP, DNP, MBA; Maneesh Batra, MD, MPH; Elena Bosque PhD, ARNP, NNP‐BC; Sara Berkelhamer, MD.
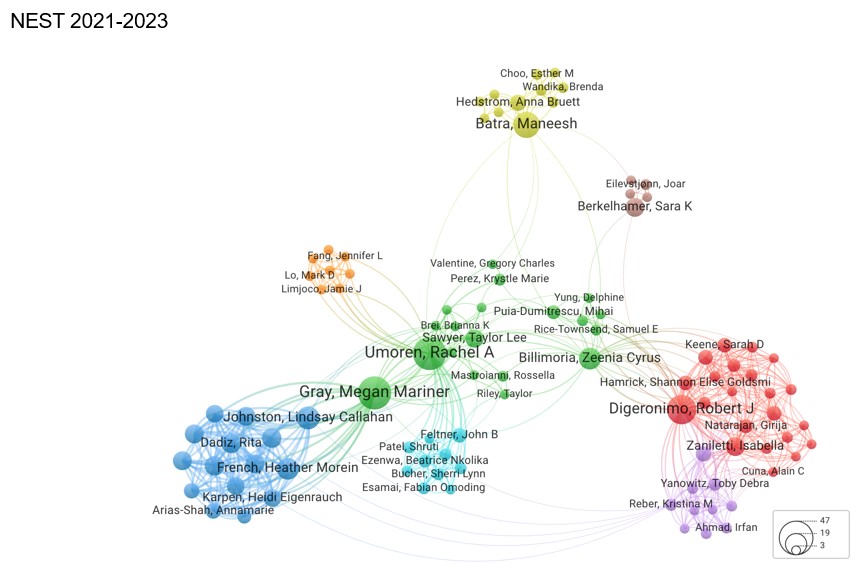
In 2014, the Division of Neonatology joined an elite group of neonatal divisions by establishing a dedicated neonatal simulation program. The Neonatal Education and Simulation‐ based Training (NEST) Program sets the UW and Seattle Children’s Division of Neonatology apart and highlights the Division’s dedication to simulation‐based education. The mission of the NEST Program is to improve neonatal outcomes through advanced technology‐enhanced training and simulation research. The program’s vision is to provide global leadership in neonatal education, simulation‐based training and scholarship.
Current projects include: ‘boot camps’ for residents and fellows, neonatal resuscitation training, neonatal procedural skills training, computer‐based and virtual reality simulators in neonatal resuscitation, prenatal counseling and disaster preparedness. The NEST program works to improve the care of neonates in the Seattle region and beyond through educational outreach with neonatal care providers and transport teams.
- Translational, Clinical, and Quality Improvement Research
Zeenia Billimoria, MD; Shilpi Chabra, MD; Robert DiGeronimo, MD; Kendell German, MD; MD; Elizabeth Jacobson, MD; Sandra Juul, MD, PhD; Dennis Mayock, MD; Ulrike Mietzsch, MD; Mihai Puia‐Dumitrescu, MD, MPH; Taylor Sawyer, DO, MEd; Thomas Strandjord, MD; Rachel Umoren, MD, MS; Elliott Weiss, MD, MSME; Steve Welty, MD
The Outcomes Research Collaborative is dedicated to improving the health and healthcare received by neonates in our units locally, regionally and nationally. Our diverse group performs innovative research in the fields of neonatal epidemiology and pharmacoepidemiology, health services research studying the impact of variation in clinical practice and outcomes, resource utilization and disparities in perinatal and neonatal healthcare. We develop and perform research projects and studies through our active affiliations with the Children’s Hospitals Neonatal Consortium (CHNC) and the Vermont Oxford Network (VON). We participate and lead pharmaceutical trials for new drugs and devices. We utilize large regional and national datasets to study short‐ and long‐term outcomes on neonates.
Our division has established a local Quality Improvement Microsystem at Children’s and a larger Regional Quality Improvement Program that oversees collaborative QI work done across all our NICUs in the region.
As practicing physicians, we always prioritize the patient. Our group conducts innovative research to deliver on our mission to share knowledge that improves the outstanding evidence‐based care of patients in our units and outside, and to educate the next generation of clinicians and researchers. This is possible through high quality translational, clinical and QI research. One of the goals of our group is to improve neonatal and pediatric therapeutics by establishing proper guidelines, dosing, safety, and efficacy of drugs and devices used in infants and children through research in pharmacotherapy, trials, and pharmacoepidemiology. We develop and perform research projects and studies through our active affiliations with the Children’s Hospitals Neonatal Consortium and the Vermont Oxford Network. We participate and lead pharmaceutical trials for new drugs and devices. We also report short‐ and long‐ term outcomes on neonates’ and infants’ data captured by different local, regional, national and international datasets that are available to us.
With the most vulnerable patient in mind (the premature infant or critically ill neonate), we are committed to translating scientific evidence into practical guidelines and establishing new therapies and treatment standards for the ultimate goal of improving the lives of our patients.
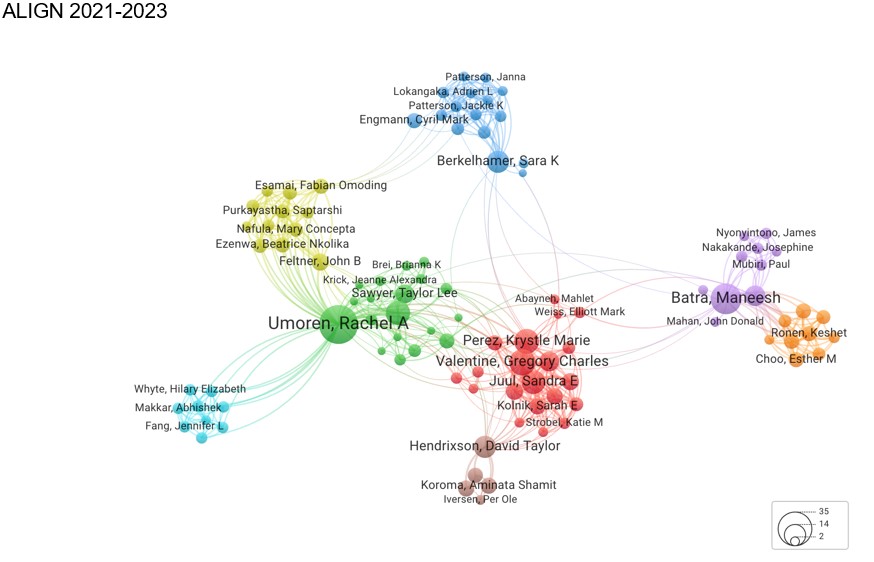
- Global Neonatal Medicine (ALIGN)
Maneesh Batra MD MPH, Sara Berkelhamer MD, Cyril Engmann MD, Anna Hedstrom MD, Krystle Perez MD MPH, Rachel Umoren MBBCh, MS, Gregory Valentine, MD MEd
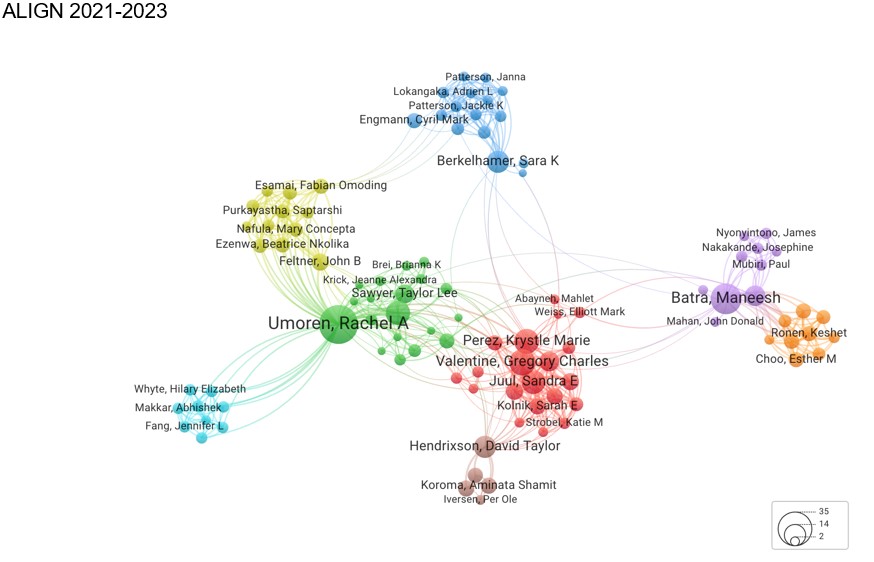
We have a focus on improving neonatal outcomes globally. The majority of small and sick newborns are born in resource‐limited settings where there are significant barriers to optimizing neonatal care. Additionally, a significant proportion of newborns in these settings are at risk for not meeting their developmental potential. Our members have a focus on overcoming these barriers through various means: advocacy and policy changes at local, national, and international levels; development of low‐cost, innovative solutions to resource‐constraints; mentorship for trainees seeking global health educational opportunities; and research into the impact of health disparities and how resource‐allocation impacts both maternal and neonatal outcomes. In 2020, our group developed ALIGN (Advancing Learning and Innovation in Global Neonatology) to enhance collaboration among members both within and outside of our division. The goal is to facilitate and promote projects that focus on improving neonatal outcomes and health disparities both locally and worldwide.
- Neonatal Ethics and Parental Decision-Making
Track Director: Elliott M Weiss, MD, MSME
Faculty Mentors:
- Josie H. Amory, MD (Neonatal/Perinatal Palliative Care)
- Jori F Bogetz, MD (Division of Bioethics and Palliative Care)
- Malia Fullerton, DPhil (UW Bioethics and Humanities)
- J. Craig Jackson, MD, MHA (Neonatology/Fetal Care and Treatment Center)
- Amanda Kim, MD
- Brennan Kim, MD
- Douglas J Opel, MD, MPH (Division of General Pediatrics)
- Benjamin Wilfond, MD (Division of Pulmonology and Sleep Medicine)
Overview: The Division of Neonatology has been highly active in bioethics scholarship through division members and through collaborations with scholars from the University of Washington Department of Bioethics and Humanities Treuman Katz Center for Pediatric Bioethics & Palliative Care. Fellows participating in the Neonatal Bioethics Track will have the opportunity to conduct research in bioethics related to neonatal care and will be able to take advantage of the outstanding bioethical resources at the University of Washington and Seattle Children’s Hospital. Research methodologies include qualitative interviews, quantitative surveys, case studies, and conceptual work. Fellows may apply for the Treuman Katz Bioethics Fellowship, a unique opportunity which includes mentored scholarship, education, and ethics consultation experience, as well as formal coursework towards a Master’s in Bioethics. This will prepare them well for a career in academic neonatal bioethics.
Current Projects:
- Supporting parental decision-making in the NICU
- Research participation in the NICU
- Use of biases and heuristics in medical decision-making
- Models of shared decision-making
- Neuroethics, including caring for infants with severe neurological impairment
- Ethics of perinatal consultation
Track Opportunities:
- Concurrent Clinical Bioethics Fellowship through the Treuman Katz Center for Pediatric Bioethics & Palliative Care
- Attendance at the Annual Pediatric Bioethics Conference
- Graduate level coursework in bioethics
- Clinical ethics consultation experience
- Research ethics consultation experience
- Hospital ethics committee involvement
- Participation in combined Neonatal-Obstetric ethics conferences
- Counseling prenatal clinic patients with life-threatening fetal conditions under the mentorship of a Fetal Center neonatologist
- Neonatal Pulmonary Physiology
Sara Berkelhamer, MD
The complex physiology of premature and newborn infants represent an area of great interest in optimizing outcomes. Despite notable progress in both survival and associated morbidity with premature birth, limited progress has been made in reducing rates of bronchopulmonary dysplasia. Research in translation models of pulmonary disease provide insight into basic mechanisms and optimal management of disease. Novel work in resuscitation models influences resuscitation algorithms at birth.
- Microbial Interactions and Nutrition and Development (MIND)
Katie Strobel (Director), Agnes Chao, Taylor Hendrixson, Rebecca Hoban, Sunny Juul, Krystle Perez, Greg Valentine, and Tommy Wood
This is a research and quality improvement group of individuals interested in parent-infant nutrition, human milk, and multi-omic systems biology approaches. The research performed includes animal models, translational research, and clinical research locally and internationally. Sessions consist of QI, research project, or grant overview and feedback, scientific writing reviews, and journal clubs.
Areas of Focus:
Examining birthing parent health and perinatal outcomes: Parent health is a critical aspect of fetal-infant growth and nutrition and the developing microbiome. Our team is interested in parental inputs such as stress, HIV, oral health, and nutritional status and its influence on both pregnancy and neonatal outcomes.
Optimizing human milk (HM) production, use, and equitable access: Our research group believes HM is more than food, but a bioactive system that all infants should have the opportunity to receive. Our work in HM spans advocacy at the state level, animal models, biomarker investigation, and clinical trials in both infants and lactating parents.
Fetal to neonatal transitional nutrition and growth: The fetal-to-neonatal transition period can place vulnerable infants at risk for nutrient deficits, growth faltering, and altered neurodevelopment. Our research group focuses on improving our understanding of growth and the use of modern technologies to assess growth and body composition. Our group also studies the prevention of nutrient deficits by appropriate fluid management, electrolyte management, and iron sufficiency.
- Congenital Diaphragmatic Hernia (CDH)
Details Coming Soon.
- Neonatal-Perinatal Fellowship Training Program
Megan Gray, MD, Program Director
Kendell R. German, MD, Associate Program DirectorThe Neonatal‐Perinatal Medicine Fellowship Training Program at the University of Washington began in the mid‐1960s. Our mission is to educate and inspire the next generation of neonatologists who will provide state‐of‐the‐art, evidence‐based clinical care, and to assist and mentor them in finding and pursuing their scholarly passion so they are poised to be the future academic leaders of our field. Read more about our fellowship at our Neonatal-Perinatal Fellowship webpage.
- Resident Education
Krystle Perez, MD, MPH, Associate Director, Pediatric Residency Program
Our faculty, fellows, and advanced neonatal practitioners are involved in several aspects of the core training program for pediatric residents. Currently the University of Washington Pediatric Residency Program accepts 45 residents per year. All residents complete one 4‐week rotation in the UWMC NICU during their intern year and one or more rotations in the UWMC NICU and SCH NICU over the course of their subsequent 2 years of residency. For all of these trainees our faculty, fellows and advance neonatal practitioners provide bedside teaching during the rotation. Additionally, our Division has been responsible for training all pediatric interns in the Newborn Resuscitation Program (NRP). Several of our faculty are invited to participate each year in the WWAMI (Washington, Wyoming, Alaska, Montana, and Idaho) visiting professor program. Our neonatologists and neonatal APPs are involved in the training of Family Practice residents at several of our clinical sites.
- Medical Student Education
Kirti Upadhyay, Course Director
An elective rotation in the UWMC NICU is offered to 4th year medical students. Division faculty also lecture in various medical school courses (for example, Ethics) and offer research experience for students in their laboratories. In addition, selected faculty have participated in the University of Washington’s medical school “College Faculty” program.
- Advanced Practice Provider Training
Elena Bosque, PhD, NNP, Neonatal Program Development
We have developed a two‐pronged approach to grow the neonatal advanced practice provider (APP) staff in our many hospitals:
- Neonatal Physician Assistant (PA) Fellowship Program: A 12‐month neonatal PA fellowship program included clinical training and weekly didactics. Case‐based presentations were provided by neonatal APPs, neonatologists, and allied professionals.
- New Graduate Nurse Practitioner (NNP) Orientation Program: The new graduate NNP program included clinical training and monthly meetings with peer support, lectures, and case presentations. For both programs, neonatal APP’s are clinical mentors. Team‐building activities supported mentorship and collaboration among all care providers.
Over 50 neonatal SCH APPs provide mid‐level care in seven Level II‐IV NICUs in the region, in collaboration with UW/SCH neonatologists. They support the training of UW pediatric residents and family practice residents in the region, educate nurses, participate in quality improvement projects and champion research.
In addition, the SCH NNPs train NNP students from long‐distance Masters/Doctorate in Nursing Practice NNP Programs from around the country.
- Continuing Faculty Education
- Weekly: UWMC and community sites BPD team conference; Fellows’ clinical conference/board review for fellows and faculty; Conference, rotating agenda for clinical, research, education, business topics; Bedside SCH NICU clinical conference with pediatric surgeons; Bedside SCH Neurosurgery teaching rounds; SCH BPD team conference; Prenatal genetics and imaging conference; Research conference; SCH Neuro‐NICU conference; SCH NICU Radiology teaching conference; Department of OB/GYN Grand Rounds, Department of Medicine Grand Rounds, Department of OB/GYN Grand Rounds
- Monthly: Neonatology/Surgery clinical conference; SCH Neonatal Neuroradiology conference
- David E. Woodrum Faculty Teaching Award
 Each year, UW Medicine's Department of Pediatrics Neonatology recognizes one individual in the division for outstanding teaching and mentoring of neonatal fellows. You may donate to the David E. Woodrum Faculty Teaching Award.
Each year, UW Medicine's Department of Pediatrics Neonatology recognizes one individual in the division for outstanding teaching and mentoring of neonatal fellows. You may donate to the David E. Woodrum Faculty Teaching Award.Past Winners:
- 2024: Sara Berkelhamer, MD
- 2023: Greg Valentine, MD, Med
- 2022: Megan Gray, MD
- 2021: Maneesh Batra, MD, MPH
- 2020: Mihai Puia Dumitrescu, MD, MPH
- 2019: Anna Hedstrom, MD
- 2018: Zeenia Billimoria, MD
- 2017: Shilpi Chabra, MD
- 2016: Kendra Smith, MD
- 2015: Paul Mann, MD
- 2014: Michael D. Neufeld, MD, MPH
- 2013: Christopher M. Traudt, MD
- 2012: Dennis Mayock, MD
Taylor L Sawyer, DO, MEd, MBA
Division Head and William Alan Hodson Endowed Chair of Neonatology Professor
Rachel A Umoren, MB, ChB, MS
Professor Associate Division Head, Research Medical Director, Inpatient Telehealth, Seattle Children’s Hospital Adjunct Professor, Division of Healthcare Simulation Science & Department of Global Health
Megan Mariner Gray, MD
Associate Professor Program Director, Neonatal‐Perinatal Medicine Fellowship Training Program Associate Division Head of Education Co-Director, NEST Program
Christina M Long, DO
Clinical Professor Associate Division Head, Clinical Operations Medical Director, NICU, Valley Medical Center Director of Newborn Services, Valley Medical Center Chief, Department of Pediatrics, Valley Medical Center
Ivana Brajkovic, MD, MPH
Clinical Assistant Professor Associate Division Head of Equity, Diversity, Inclusion and Anti-Racism
1959 NE Pacific St.
Box 356320, RR542 HSB
Seattle WA 98195-6320
Tel (206) 543-3200
Fax (206) 543-8926
neonatologyadmin@uw.edu






